Oral Medications: Clomid & Letrozole
These are often the first-line treatments for ovulation disorders:
- Clomid (Clomiphene Citrate)
- How it works: Blocks estrogen receptors, tricking your brain into producing more follicle-stimulating hormone (FSH) to grow eggs.
- Typical dose: 50–100 mg daily for 5 days (starting early in your cycle).
- Success: ~70–80% ovulation rate, with a 10–15% pregnancy rate per cycle (higher with IUI).
- Side effects: Mood swings, hot flashes, rare risk of thinning uterine lining with long-term use, and a rare risk of head ache and visual changes that goes away after stopping the medication.
- Letrozole (Femara)
- How it works: Temporarily lowers estrogen made in adipose tissue, prompting your body to produce more FSH naturally. it may also treat silent endometriosis.
- Often more effective than Clomid for PCOS, with higher live birth rates.
- Typical dose: 2.5–7.5 mg daily for 5 days.
- Fewer side effects than Clomid (less uterine lining thinning).
Directed Hormonal Treatments
Some women need additional medications to address underlying hormonal issues:
- Metformin for PCOS
- Improves insulin resistance, which can help restore regular ovulation.
- Often used alongside Clomid/Letrozole for better results.
- Steroids (Dexamethasone/Prednisone)
- Used if high adrenal androgens (like DHEA-S) are suppressing ovulation.
- Dopamine Agonists (Cabergoline/Bromocriptine)
- Prescribed for high prolactin levels, which can block ovulation.
Injectable Hormones (Gonadotropins)
If oral medications don’t work, FSH/LH injections may be the next step:
- How they work: Directly stimulate the ovaries to produce multiple follicles.
- Monitoring is critical: Frequent ultrasounds and blood tests prevent overstimulation (OHSS) and cancellation due to more than 1-2 eggs.
- Success rates: Higher than oral meds (~15–25% pregnancy per cycle with timed intercourse/IUI).
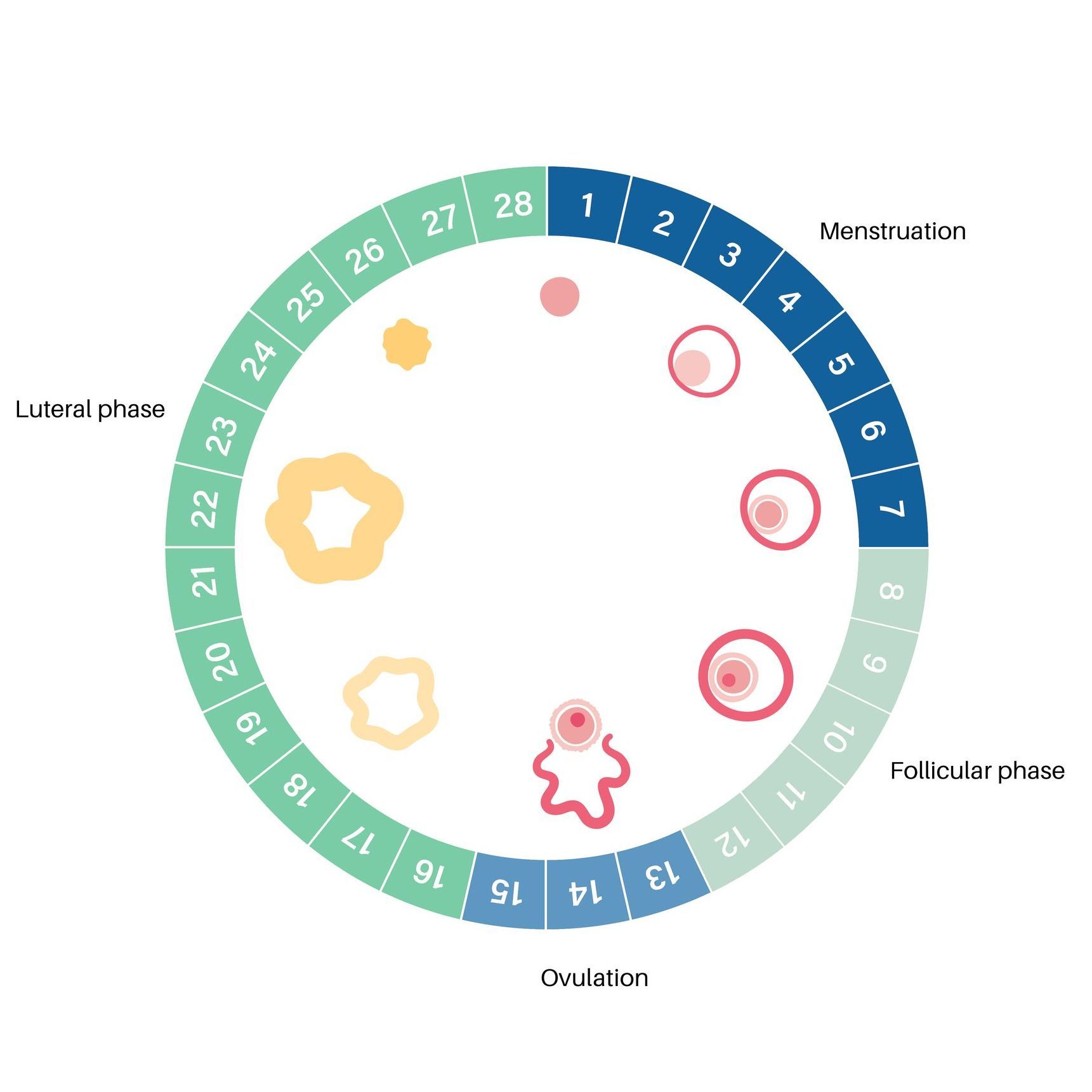
Cycle Monitoring:
Why It Matters
- Ultrasounds track follicle growth to predict ovulation timing.
- Blood tests (LH, progesterone) confirm if/when ovulation occurs.
- Trigger shots (hCG) may be used to perfectly time ovulation for IUI or intercourse.
Which Treatment Is Right for You?
The best approach depends on:
✔ Your diagnosis (PCOS, hypothalamic amenorrhea, etc.)
✔ Your response to medications (some women need dose adjustments)
✔ Your goals (trying naturally vs. combining with IUI/IVF)
Next Steps:
We will tailor a plan based on your hormones, ultrasound findings, and medical history. Many women conceive within 3–6 OI cycles—but if ovulation isn’t happening, we can discuss stronger options.
Remember: Ovulation induction is a powerful tool, but
patience and monitoring
are key. We’re here to guide you every step of the way!
Connect with us
Ready to start the treatment process?
We offer direct honest answers and explanations in a practice where you always come first.
Click the button below to schedule your initial visit.